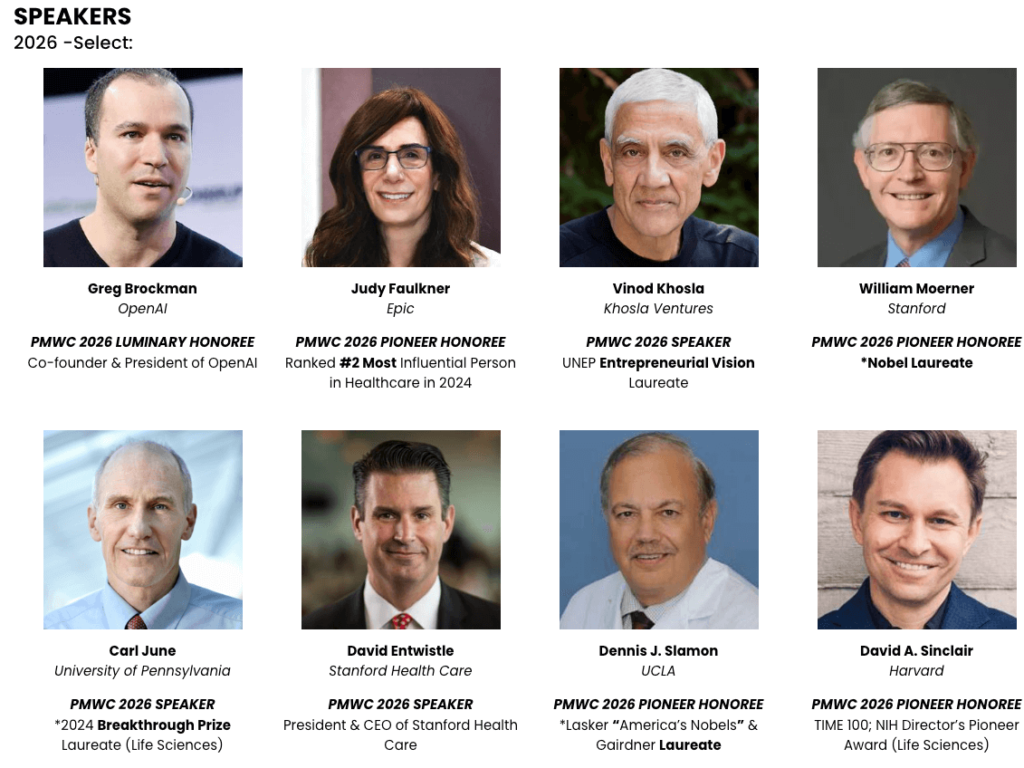




SPEAKERS / HONOREES
2026 -Select:
Co-founder & President of OpenAI
Ranked #2 Most Influential Person in Healthcare in 2024
Co-Founder of Apple
*2025 Nobel Laureate
*Nobel Laureate
President & CEO of Stanford Health Care
Co-founder & Co-CEO of Chan Zuckerberg Initiative
UNEP Entrepreneurial Vision Laureate
Led the First Human Genome Sequencing
Pioneered automated DNA sequencing and systems biology
*2024 Breakthrough Prize Laureate (Life Sciences)
TIME 100; NIH Director’s Pioneer Award (Life Sciences)

DAYS

ATTENDEES (35 COUNTRIES)

EXHIBITORS

PARALLEL TRACKS
REGISTRATION
Tickets to PMWC - Est. 2009
Loading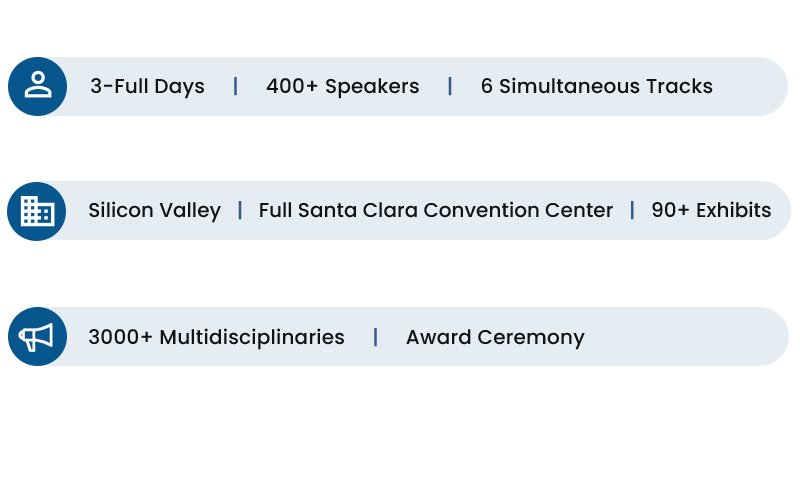

Format
The conference format consists of five parallel talks spanning 3 full days. Main Tracks 1-4 include sessions by leaders in the commercial, pharmaceutical, academic, government, regulatory, venture capital, and non-profit arenas that deliver a broad and up-to-date array of content across the various facets of precision medicine. Session discussions focus on time-relevant aspects with a selected set of key stakeholders, while commercial sessions cover the latest developments in technologies that are instrumental for the success of further adoption of precision medicine.
Additional 2 Tracks, feature Showcases: companies and research institutions can promote their platforms, launch products, and share research developments to a targeted audience – Apply.
For over a decade, PMWC has recognized individuals who have played a significant role in transforming health care by advancing precision medicine in the clinic with the Luminary and Pioneer Awards. The honorees’ numerous technological and scientific contributions have expedited this transformation as demonstrated by the clinical adoption of precision medicine, and the ongoing introductions of novel clinical applications. For a deeper look into the fascinating achievements of our past awardees see the awards page.
Receive the latest news about the field of precision medicine, and the conference from Tal Behar, PMWC’s President:
- 1. Breaking the Gene Fusion Paradigm: Your discovery of the TMPRSS2-ERG gene fusion – now recognized as a defining molecular event in prostate cancer – broke new ground by revealing that gene fusions can drive common solid tumors. Could you share how this landmark finding has influenced prostate cancer care (for example, in developing new diagnostic tests or targeted therapies) and what it taught researchers about the importance of genomic subtyping in cancer?
- 2. Translating Genomics to Therapy Decisions: You have been a leader in precision oncology, integrating comprehensive DNA and RNA sequencing of patient tumors into treatment decisions since as early as 2011 through programs like Mi-ONCOSEQ Could you describe a specific case where this integrative approach uncovered an unexpected cancer driver (such as a gene fusion or mutation) and guided a patient’s therapy, and what this illustrates about the value of multi-dimensional genomic data in managing advanced cancers?
- 3 Beyond DNA – The Multi-Omics Frontier: The field is now moving beyond DNA variants into “multi-omics” approaches for monitoring and treating cancer. How do you envision integrating additional data layers – such as transcriptomics (RNA), epigenetic markers (e.g. DNA methylation), proteomics, or liquid biopsy readouts – into precision oncology? For example, what emerging multi-omic strategy do you find most promising for improving early detection or real-time monitoring of cancer (like minimal residual disease) and guiding therapy decisions in ways that single-modality genomic tests cannot?
- 07 Dec ,2025
Precision Medicine World Conference
Jeff Balser Interview
1. AI / operations
VUMC’s strategy is to use AI to scale as a means to grow while better controlling increases in staffing. In what areas are you focusing?
Our approach is to focus on specific domains while developing standard platforms and processes to facilitate AI implementation across many domains. Most of the opportunities we are exploring are not directly in the patient-clinician interaction, but rather are aimed at expediting the vast array of tasks that surround those interactions. Key areas of focus include:
1) Revenue Cycle – Opportunities range from preauthorization to documentation. Our efforts in these areas emphasize augmenting the productivity of the individuals performing these tasks. For example, we are using AI to prompt our clinicians to consider diagnoses they might have missed, or to provide our clinical teams with all the necessary information in a consistent and comprehensive format for submitting a preauthorization request. This cuts down on the need for multiple submissions and phone calls with incomplete information.
2) Ambulatory Care – Opportunities range from front-desk to back-office tasks. We are preparing to pilot a “clinic of the future” designed to minimize staffing needs beyond the clinician and the patient. This requires standardizing the vast array of clinic processes so they are “computable,” such as preregistration questions and prescription refills. Much of our work in AI implementation involves standardizing processes to make them computable. This is a culture challenge in many clinical practices, particularly academic practices.
There is growing evidence that forms of agentic AI are well accepted or even preferred by consumers. We are exploring the use of avatars for scheduling, greeting, collecting information, verifying data, and navigating clinic patients through their care experience. These will be implemented through staged pilots to better understand what patients and care providers like and dislike, so we can tune the process for the best outcomes.
While there is work on the use of AI in the direct clinician-patient interaction, that’s an even greater challenge. We have plenty of important work to do that will dramatically improve the patient experience that doesn’t involve the clinician – patient interaction. The aspects of clinical care that we are prioritizing should look and feel like other kinds of consumer experiences. Healthcare has underperformed in these areas, and AI gives us a chance to catch up.
2. AI / adoption at the point of care
DAX Copilot is rolling out across Vanderbilt to cut documentation burden. What specialty or care setting will benefit most? How will you measure success?
We participated in pilot phases of the Dax Copilot development and are now one of the largest implementations, with over 1,400 clinicians using the tool across nearly every specialty in the ambulatory setting. It’s too early to know whether some specialties have better outcomes than others, but we are so encouraged by the early results we are now expanding its use to inpatient activities, including bedside care documentation for nursing.
To evaluate impact, we are tracking several key metrics:
· Improvement in clinician burnout – We are already seeing a reduction in burnout scores in our faculty Mini Z survey.
· Enhanced patient experience – This is reflected in higher patient satisfaction scores and the feedback we hear from patients who feel like their clinician is more focused on them and less on a computer screen.
· Reduction in “pajama time” – Our clinicians are reporting that they are spending less time doing after-hours chart documentation.
· Increased clinical throughput – We are seeing an increase in visits per day for clinicians who have adopted the technology.
Over the past 20 years, no advance in electronic health record use has had as great an impact on clinician satisfaction as this. As a very large training center, we included our residents in the rollout, and not surprisingly, they are heavy adopters. I feel this fundamentally changes how we train students and residents, freeing them from the keyboard distraction during their interactions with patients.
3. Genomics / clinical impact (AGD)
AGD has completed 280,000 whole genomes from BioVU, with multi-omics coming next. Illumina and 9 pharma/biotech companies financed this sequencing at a cost of well over $100 million – so they must have believed this would be incredibly valuable for drug discovery. Can you elaborate on what you believe will be some of the early wins? And are there any opportunities for VUMC to utilize the resource in patient care?
There are a number of ways these whole genomes are likely to move us forward. Keep in mind that the phenotypic information in BioVU is constantly updated, and has been for nearly 20 years, so the clinical context is a movie, not the snapshot that many other DNA banks provide. Given our past work was based on genotyping arrays rather than WGS, we can anticipate, with whole genomes in hand, the discovery of a host of new loss- or gain-of-function mutations that essentially act as natural drug experiments. These could range from inflammation and immune dysregulation to cardiometabolic pathways, to neurodegeneration and neurologic disease.
One approach for querying this kind of data developed at VUMC is PheWAS, essentially the inverse of GWAS. Given this is our first use of PheWAS in a large-scale WGS cohort, we expect to identify numerous biologically distinct disease subgroups, enabling targeted drug development or repurposing opportunities. We are also likely to see opportunities to precisely identify drug side effects, far earlier in the drug-discovery process, allowing clinical trials to be more targeted to the right populations, or avoided altogether.
Finally, there are direct opportunities to use the resource in patient care. VUMC is a national leader within the NIH Undiagnosed Diseases Network (UDN) with a multidisciplinary team integrating clinical genetics and a host of medical specialties with BioVU’s large genomic and phenomic resource, coupled to AI-supervised diagnostic pipelines. One way that BioVU is used in the UDN is “patients like me” matching – not only individuals with the same rare variant, but individuals with similar gene variant patterns, or with shared phenotypes in the EHR.
VUMC platform delivers a 62% diagnostic yield, far above national benchmarks, as well as shorter time-to-diagnosis, and reduced redundant testing, consults, imaging, and admissions. We are expanding access to the program far beyond the NIH-supported level, with a goal to reach 1000 patients annually over the next few years.
4. Genomics / governance
Moving AGD from an academic resource to a global drug-discovery engine raised big governance questions. Describe challenging ethical or data-use hurdles, and how did you solve them?
An overarching challenge in leveraging BioVU for drug discovery involving the commercial sector was establishing a governance model that honored the academic and ethical roots of BioVU, which was built over decades of trust with our patients, while also supporting responsible use of the data to help develop new treatments and diagnostics.
Reaching the right balance surrounding the protection of de-identified clinical and genetic information was fundamental. Our approach involves having the AGD datasets housed only in protected bioinformatics workspaces called Trusted Research Environments, or TREs – think of these as cyber vaults that are heavily monitored and audited to establish, and maintain, trust. Egress of summary data and scientific results from these environments is allowed, but individual, subject-level data cannot be removed.
While there are many other safeguards, a major one is that all of the clinical data in BioVU is deidentified, unlike many DNA banks. It should also be noted that we only provide discrete (structured) data fields from our de-identified health records to match to whole genome sequencing for AGD use – and that’s been our approach for many years in our ongoing work with industry using BioVU. As such, the reidentification risk is much lower than with more narrative data from EHR content such as progress notes. Access to the more narrative information is possible, and incredibly valuable for R&D use, but industry must work directly with VUMC and its subsidiary, NashBio, to access that more nuanced, unstructured information.
- 05 Dec ,2025
Q1. What impact is Dragon Copilot having today, and what outcomes are you prioritising for 2026?
A1. Dragon Copilot gives clinicians time back and reduces cognitive burden—shifting focus from paperwork to patients.What began with physicians now increasingly supports nurses and radiologists. In 2026, we’ll continue expanding to additional care teams while simplifying workflows to reduce administrative load and improve productivity.Our focus remains the same: outcomes. Clinicians report a 70% improvement in work–life balance and meaningful reductions in burnout and fatigue. And 93% of patients say their clinician is more personable and conversational when using our technology.The work ahead is scale—bringing these gains to more care teams and enabling the broader ecosystem at this shared AI frontier.To support that ecosystem, we’re introducing new extensibility capabilities in Dragon Copilot. Partners can now build and deploy AI applications and agents directly within the Dragon Copilot experience.This strengthens clinical intelligence at the point of care, maintains workflow continuity, and accelerates responsible innovation across healthcare.
Q2. Which integrations and guardrails matter most for deploying ambient AI across health systems?
A2. Integration is the backbone of a seamless clinical experience. Our partner ecosystem of EHR providers, ISVs, system integrators, and cloud service providers each plays a distinct role in helping health systems procure, deploy, and scale ambient AI.Guardrails begin with a secure data estate. Layered on top are healthcare-specific clinical, conversational, and compliance safeguards that ensure accurate and safe AI outputs. We do not compromise here. Every deployment is guided by Microsoft’s Responsible AI Standard and principles of fairness, reliability and safety, privacy and security, transparency, accountability, and inclusiveness.These guardrails help health systems evaluate and mitigate risks, ensure compliance with HIPAA and other regulations, and maintain trust with patients and providers.
Q3. Can you share one commitment Microsoft is making in 2026 that advances precision medicine at scale, and one dependency that must be true to realize it
A3. Medicine is iterative. No one walks into the clinic and has every question answered at once. Colleagues in Microsoft AI are exploring how MAI-DxO’s multimodal, sequential diagnostic reasoning could strengthen the foundations of precision medicine by helping clinicians identify the right next question or test and integrate signals across imaging, labs, notes, and longitudinal history. The aim is to surface risk earlier, reduce low-value testing, and better align diagnostic and treatment decisions to the individual patient.A key dependency for anyone innovating in this space is continued progress on interoperability and secure, trusted data exchange, so that advanced reasoning systems can operate on high-quality clinical data within strong privacy, safety, and governance frameworks.
- 25 Nov ,2025