



SPEAKERS / HONOREES
2026 -Select:
Co-founder & President of OpenAI
Ranked #2 Most Influential Person in Healthcare in 2024
Co-Founder of Apple
*2025 Nobel Laureate
*Nobel Laureate
President & CEO of Stanford Health Care
Co-founder & Co-CEO of Chan Zuckerberg Initiative
UNEP Entrepreneurial Vision Laureate
Led the First Human Genome Sequencing
Pioneered automated DNA sequencing and systems biology
*2024 Breakthrough Prize Laureate (Life Sciences)
TIME 100; NIH Director’s Pioneer Award (Life Sciences)
15-MINUTE PRESENTATIONS
AUDIENCE: UP TO 200 INVESTORS, POTENTIAL CLIENTS AND PARTNERS
Apply by !
The Foremost Precision Medicine Conference
• Gathering recognized leaders, top global researchers and medical professionals, plus innovators across healthcare and biotechnology sectors
• Showcasing latest practical content that helps close the knowledge gap among different sectors
• Promoting cross-functional fertilization & collaboration to accelerate Precision Medicine
• Main Tracks and Showcases (6 Total) that provide a mix of established and upcoming perspectives
• Luminary and Pioneer Award Ceremony honoring those who transform healthcare by advancing precision medicine in the clinic
PMWC provides a valuable insight for physicians and others who may be wondering how close we are getting to realizing the arrival of personalized medicine. The conferences are helpful in understanding where and how the envelope is being pushed.
Peter Paul Yu, MD, FACP, FASCO, Immediate Past President, ASCO
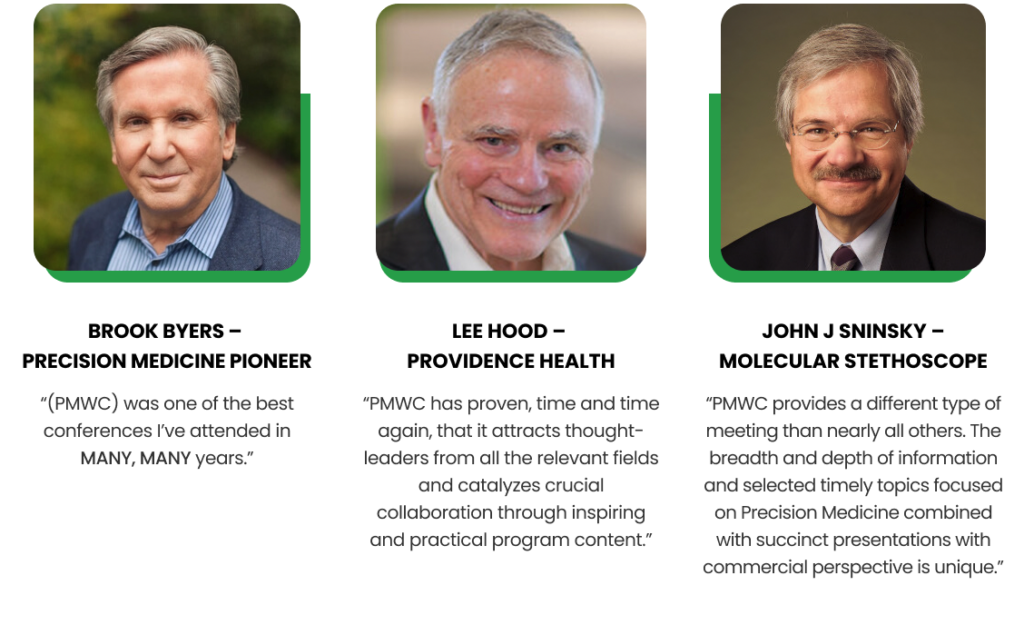
PMWC has proven, time and time again, that it attracts thought-leaders from all the relevant fields and catalyzes crucial collaboration through inspiring and practical program content. This is the Conference for entrepreneurs to meet payors, and for researchers to connect with service providers and for clinicians to hear from leading providers.
Lee Hood, PhD, MD, President, Institute for Systems Biology

DAYS

ATTENDEES (35 COUNTRIES)

EXHIBITORS

PARALLEL TRACKS
REGISTRATION
Tickets to PMWC - Est. 2009
Loading

PMWC Overview
PMWC, the “Precision Medicine World Conference” is the largest & original annual conference dedicated to precision medicine. PMWC’s mission is to bring together recognized leaders, top global researchers and medical professionals, and innovators across healthcare and biotechnology sectors to showcase practical content that helps close the knowledge gap between different sectors, thereby catalyzing cross-functional fertilization & collaboration in an effort to accelerate the development and spread of precision medicine.
Since 2009, recognized as a vital cornerstone for all constituents of the health care and biotechnology community, PMWC provides an exceptional forum for the exchange of information about the latest advances in technology (e.g. DNA sequencing technology), in clinical implementation (e.g. cancer and beyond), research, and in all aspects related to the regulatory and reimbursement sectors.
Testimonials
Format
The conference format consists of five parallel talks spanning 3 full days. Main Tracks 1-4 include sessions by leaders in the commercial, pharmaceutical, academic, government, regulatory, venture capital, and non-profit arenas that deliver a broad and up-to-date array of content across the various facets of precision medicine. Session discussions focus on time-relevant aspects with a selected set of key stakeholders, while commercial sessions cover the latest developments in technologies that are instrumental for the success of further adoption of precision medicine.
Additional 2 Tracks, feature Showcases: companies and research institutions can promote their platforms, launch products, and share research developments to a targeted audience – Apply.
For over a decade, PMWC has recognized individuals who have played a significant role in transforming health care by advancing precision medicine in the clinic with the Luminary and Pioneer Awards. The honorees’ numerous technological and scientific contributions have expedited this transformation as demonstrated by the clinical adoption of precision medicine, and the ongoing introductions of novel clinical applications. For a deeper look into the fascinating achievements of our past awardees see the awards page.
Receive the latest news about the field of precision medicine and the conference from Tal Behar, PMWC’s President:
Interview with Tal Zaks, Partner, OrbiMed Advisors LLC
Tal Zaks, Partner, OrbiMed Advisors LLC
Topic: Personalized mRNA cancer vaccines, ROI realities, and what it takes to win in oncology beyond the COVID playbook
1
ROI Black Holes: Where the probability of success is won or lost
The blunt point: ROI follows clinical success, and cancer vaccines have a long history of “great story, zero payoff.” Tal explains why the Moderna PCV data in melanoma is different, and why trial design is the real lever.
So why is this time different and I'm referring to the randomized phase 2 an adjuvant melanoma of Moderna's personalized cancer vaccine. I think for three reasons. First, is that we've learned that when the immune system does see an antigen in the context of cancer, it is far far more likely to be a neo epitope than it is to be encoded by a non-mutated protein. And we now have both the sequencing tools and bond for attic tools to be able to quickly analyze a patient's tumor for those new epitopes that are most likely to bind to that patient's HLA.
The second is that mRNA vaccine provide a uniquely potent T cell vaccine. It is worth noting that this is not by our clever design but rather by evolution. When you concatenate 30 or more short peptides and one long mRNA chain, what comes off the ribosome is a misfolded protein that you would expect get preferentially shuttle to the protozoal machinery and displayed for recognition because this is how the immune system has evolved T cells to recognize RNA virally infected cell cells.
Recognizing these two points and the complete lack of predictability of urine models when it comes to cancer vaccines is why we advanced Moderna's cancer vaccine to the clinic without attempting to cure mice first finally, the third factor is the clinical context. We very carefully chose the first study to be an adjuvant melanoma in combination with Keytruda. The heavier, mutation burden in melanoma suggests that it is the place where we are most likely to pick up relevant new epitopes; the proven activity of Keytruda in adjuvant melanoma combined with solid pre-clinical data suggesting that PD one blockade can enhance vaccination made this the obvious combination.
Finally, treatment in the edge of event, setting provides us with the smallest tumor burden, and the longest time window during which we can prime, boost and further stimulate an immune response. If you look at the history of developing cancer medicines, every medicine that ever worked in late metastatic disease works better the earlier you go. So coming back to your question, I think the clinical trial design is a big factor in terms of having a higher probability of success, and therefore providing a positive return on investment. By extension, I am much more hesitant to predict the utility of a personalized cancer vaccine, even if combined with a checkpoint inhibitor, in later stage metastatic, epithelial tumors. I think this has been born out, even in melanoma by some of the competitors trials.
If one desires, a positive return on investment, one should conduct a definitive experiment in the context where it is most likely to give a positive answer. That means a randomized phase 2, rather than a phase 1, when combining with another medication and studying at the adjuvant rather than the metastatic setting.
I think both the manufacturing and logistics are no longer an issue. These were significant challenges when we started back in 2015 but based on the success of mRNA vaccines for infectious disease as well as the investment that have put into improving the manufacturing footprint. At this point, this should not be an impediment for a personalized cancer vaccine to provide a solid business case for Moderna. That said this, of course, is true for Moderna and maybe Biontech, but would be a challenge for any newcomer to the field, who would need to consider the costs of CMC in their overall ROI.
Logistics are even simpler. I don't want to trivialize this as it requires very careful and close coordination between the treating centers, the sequencing and bond for Matic analysis, and the manufacturer. At a high level, in an era where we can provide personalized cell therapy, a personalized vaccine is much easier by comparison.
2
The Moderna Arc: Why COVID speed does not copy paste into oncology
If someone tells you they will “do oncology like COVID,” they are either fundraising or hallucinating. Tal breaks down what actually made the COVID timeline possible, and what does not translate when endpoints take years.
1. The first is that we had the technology from a CMC and manufacturing standpoint to go very quickly from the initial designed phase to the start of a phase 1 trial. This was a function of previous investments in the mRNA platform and can't really be replicated from a standing start. People forget that it took us eight years to get to January 2020. During that time we had tried to immunize humans in clinical trials against a different viruses. Our success rate was eight out of eight. So COVID-19 was our ninth virus. And the investment in CMC and manufacturing accelerated in the early part of 2022, match the clinical development timelines and ultimately global deployment
2. The second was close regulatory support, and guidance to move from phase one to phase 3. And disregard, I think we're seeing US biotechs learning to leverage places in the world where the regulatory framework is much more agile and quick to start, such as Australia and even China.
3. The final determination of timeline as it is for any phase 3 trial, is how quickly do you see endpoints. If you look at the original COVID-19 protocol, we thought it would take us 12 months to reach the number of events required to demonstrate efficacy. As it happened, the infectious rates across the US during the summer of 2020 were horrendous, but in a way that enabled us to reach our endpoints, i.e. cases on controls versus placebo, much quicker. 11 is winning studies and cancer gear towards overall survival, thankfully from a patient's perspective the endpoints take a long time. In fact with more and more available lines of therapy, these trials, especially in the earlier lines of treatment are taking longer than ever.
3
Steering Wheel vs Engine: What is still missing in cancer immunotherapy
Checkpoints changed the game, but they did not finish it. Tal lays out what is missing, why mouse models keep failing us, and why biomarkers are still the annoying unsolved homework.
Since the amazing success of the first checkpoint inhibitors, we as a field have spent billions trying to find the next ones, with little to show for these efforts. Except maybe the realization that there is only so much we can learn from mouse biology.
I very much hope that this first personalized cancer vaccine will in fact be positive in the phase 3 that has now completed enrollment. I am also hopeful that there will be ways to improve on its efficacy, even by such immediate parameters as increasing the number of new epitopes and improving our ability to predict which ones are relevant within a given patients immunology and biology, without having to repeat the entire clinical development paradigm.
Finally, we need to continue to improve our methods of understanding, human immunology, and human cancer immunology from human disease. The abject failure of my models to predict the efficacy of both cancer, vaccines, and novel I owe combinations hoses a unique funding challenge that is going to be difficult to overcome because it means it is challenging to de-risk and Investmont based on pre-clinical studies.
This problem is further compounded for cancer vaccines because we continue to lack for bio markers that predict efficacy. Demonstrating one can illicit tumor active teasels in the periphery is likely important, but clearly insufficient to predict for efficacy, which has been a painful lesson over the last 30 years.
- 28 Jan ,2026
Interview with PMWC 2026 Track Chair: Edward S. Kim, MD, City of Hope
Edward S. Kim, MD, Vice Physician-in-Chief, City of Hope National Medical Center; System Director, Clinical Trials, City of Hope
Track Chair: Systems Integration & Variant Interpretation
Topic: A national clinical trials model that expands access and accelerates enrollment
1
The Model: One Hub, Many Sites
City of Hope’s approach is built around a centralized operational hub that can activate and run trials across a distributed, national footprint.
2
Why Patients Care: Access That Reaches Them
Speed matters, but access matters more. The network is designed to bring trial options closer to home, especially for communities that are typically left out.
3
Speed, Scale, and What Runs on the Network
Centralization is not just organizational, it changes the timeline: activation, enrollment, and execution can move faster across a wide geographic footprint.
4
Consistency, Differentiation, and What’s Next
A national footprint only works if quality is consistent. This model is built to standardize execution while expanding reach and portfolio breadth.
- 09 Jan ,2026
Interview with Pioneer Honoree: Dennis J. Slamon, UCLA
Keynote in Track 3 Day 2: Molecular Diversity of Human Malignacies: Diagnostic and Therapeutic Implications
1
The Future of Therapeutic Target Discovery
Dr. Slamon’s work on HER2 was a groundbreaking translation of a molecular target into a life-saving therapy. The next stage of liquid biopsy (ctDNA, fragmentomics, etc.) allows us to monitor minimal residual disease (MRD) and treatment resistance in real-time.
2
Overcoming Therapy Resistance
Dr. Slamon's pioneering work in the HR+/HER2- space, notably with CDK4/6 inhibitors (like Kisqali), has significantly improved outcomes for the largest population of breast cancer patients. However, resistance remains the biggest hurdle in extending curative outcomes.
3
Global Implementation and Access
Breakthroughs like Herceptin and ctDNA-based tools have the greatest impact when they reach patients everywhere. This question related to the final panel of Day 2 addresses "From Validation to Payment: Coverage Pathways."
- 07 Jan ,2026